
Thomas Tiennot receives the jury’s Grand Prix at i-PhD contest for his project on ultrasonic treatment of drug-resistant depression

i-PhD is a contest initiated by the French Government in 2019 and awards PhD students whose research could lead to the creation of a deeptech start-up company. Our PhD student Thomas Tiennot is not only among the awardees of 2022 edition, but he also received a Jury’s Grand Prix as a recognition of his “especially promising project” on the development of a non-invasive, ultrasound-based treatment of drug-resistant depression.
Depression affects up to 1/5 of the people at least once in their lifetime. 30% of the patients who suffer from major depressive disorders do not respond to psychotherapeutic or pharmacological treatments. Current treatments of pharmaco-resistant depression aim at modulating the activity in specific regions of the brain involved in mood disorders. Current available methods have limitations, either because they are invasive (deep-brain stimulation with implanted electrodes), or they cause adverse cognitive effects (electroconvulsive therapy), or they are too superficial to efficiently reach the regions of interest (transcranial electric or magnetic stimulation).
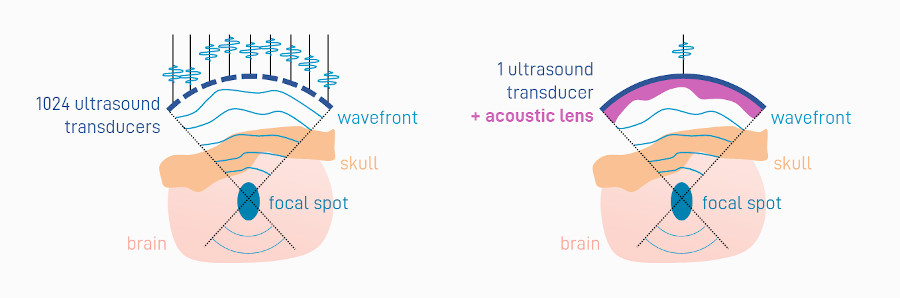
This is where ultrasound technology comes into play. Under certain settings, ultrasound waves can stimulate non-invasively (through the skull) the cerebral activity in specific regions, even deep in the brain. Controlling precisely the targeted region however requires to correct the distortions induced by the skull bone heterogeneities. Focusing ultrasound beams through the skull for therapeutic purposes has been an intensive research field for decades. Mapping the heterogeneous structure of the skull bone (e.g. using a CT scanner) enables to compute the shape of the ultrasound beam to be emitted to compensate for these heterogeneities. In practice, emitting the appropriate shape (also called ultrasound “wavefront”) can be done using different technologies. Early technologies involved ultrasound emitters consisting of hundreds of small transducers, each one sending slightly delayed ultrasound waves to produce the appropriate wavefront. Although efficient, the high number of transducers requires to use extremely costly electronics and results in cumbersome systems that are not easily translatable to clinical practice.
The innovation developed during the PhD thesis of Thomas Tiennot, under the supervision of Jean-François Aubry and Mickael Tanter at the institute Physics for Medicine Paris (Inserm, ESPCI Paris-PSL, CNRS), is a simpler system and cheaper approach with no compromise in the precision of the transcranial focusing. The researchers propose to use one large transducer only, on which they attach an acoustic lens of varying thickness to shape the emitted ultrasound wavefront. The acoustic lens is is affixed in front of the transducer and is manufactured using a 3D-printer. Its design is customized for each patient and each targeted brain area, based on previously-acquired medical images of the patients head. The developments conducted over the past three years have led to the construction of a fully-integrated device, consisting in a single-transducer with its acoustic lens, fixed on an armchair, and combined with a neuronavigator that ensures proper positioning of the transducer on the patient’s head in real time.
The next steps for Jean-François Aubry, Thomas Tiennot and their colleagues will be to validate the device on a first cohort of patients with severe depression. They plan to shortly launch a start-up company to further develop the technology. This new ultrasonic neuromodulation method might improve the management of depression in many ways. First, it offers a non-invasive solution to reach deep-seated areas in the brain with a millimetric precision. Second, the technology is cost-efficient and is therefore expected to be easily disseminated in hospitals, facilitating the access to treatment for patients. Lastly, the system is easy-to-use and hence suitable for repeated neuromodulation sessions, as needed in the treatment of drug-resistant depression.





